Case 15: A 32-Year-Old Man with Sickle Cell Disease
This 32-year-old man with sickle cell disease is seen in the hematology outpatient clinic. He has suffered from numerous episodes of sickle cell crisis. He has chronic renal insufficiency. His condition has been stable for the past 3 months: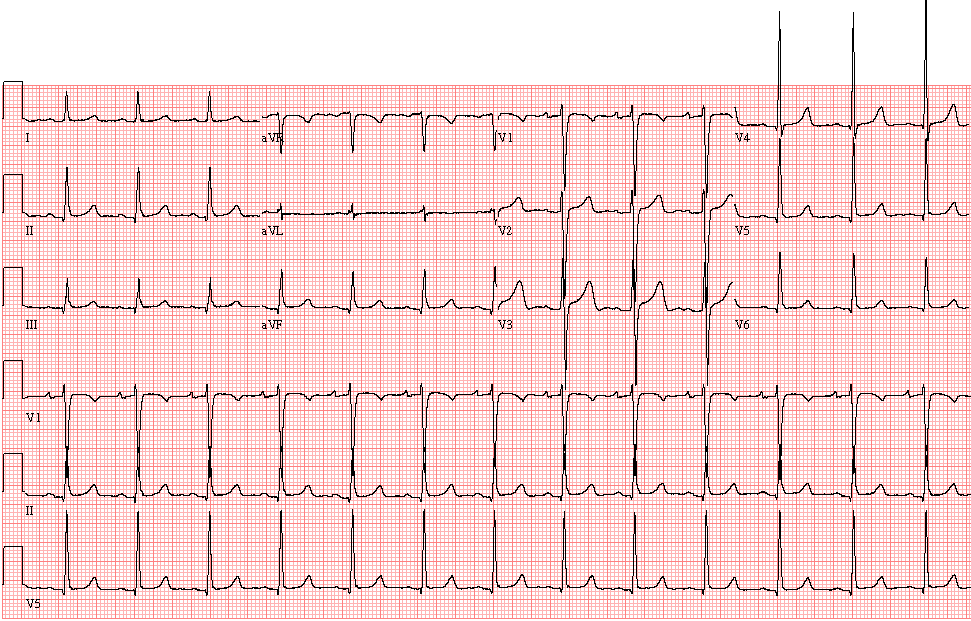
- Sinus rhythm, 79/min
- Minimal voltage criteria for left ventricula hypertrophy (SV1 + RV5 = 40 mm}
- Borderline ECG

7 days after the last clinic visit the patient is brought to the Emergency Department with a sickle cell crisis:

Compared with the previous tracing of 7 days ago, there are marked changes:
- Atrial fibrillation with rapid ventricular response (103/min)
- Right bundle branch block
- Left anterior fascicular block
- Acute anteroseptal infarction (ST elevation V1-V3 with ST depression II, III, aVF)
- Peaked T-waves (possibly related to acute infarction or hyperkalemia)
Comments: The serum potassium was found to be 7.6 mmol/L (normal 3,.5-5.1 mmol/L). The serum creatinine was 541 micromol/L (normal 52-112 micromol/L)

The following ECG is recorded 1 1/2 hour later after appropriate treatment: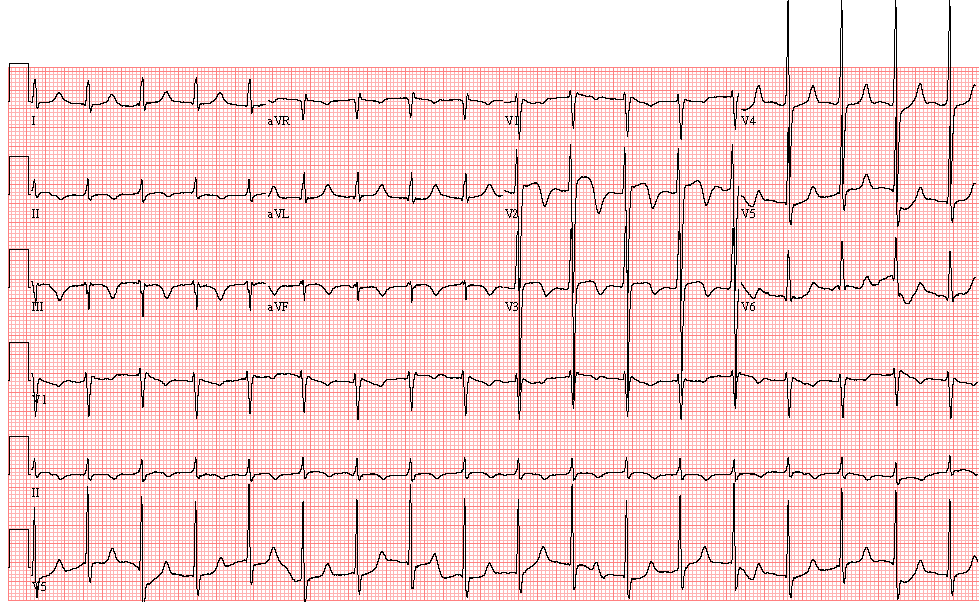
- Junctional tachycardia, 105/min
- Inferior and anterior T wave abnormality secondary to evolving changes of acute infarction
Comments:Acute hyperkalemia may occur during a sickle cell crisis, as a result of rhabdomyolysis and impaired renal function. Myocardial infarction occurs rarely with sickle crisis – vasospasm usually plays a role and thus extent of infarction is limited and conduction abnormalities usually improve rapidly following treatment.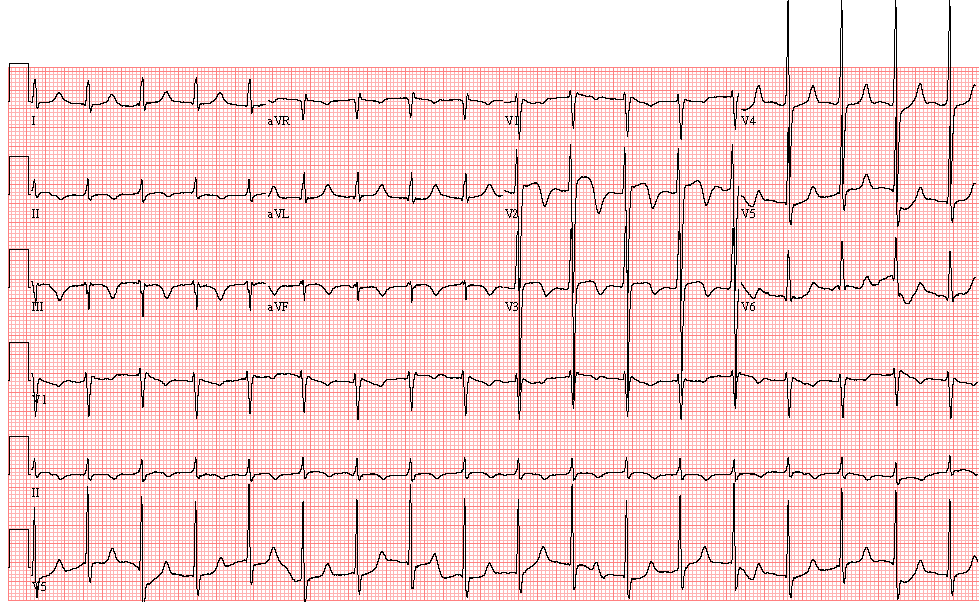
ECG ID: E671