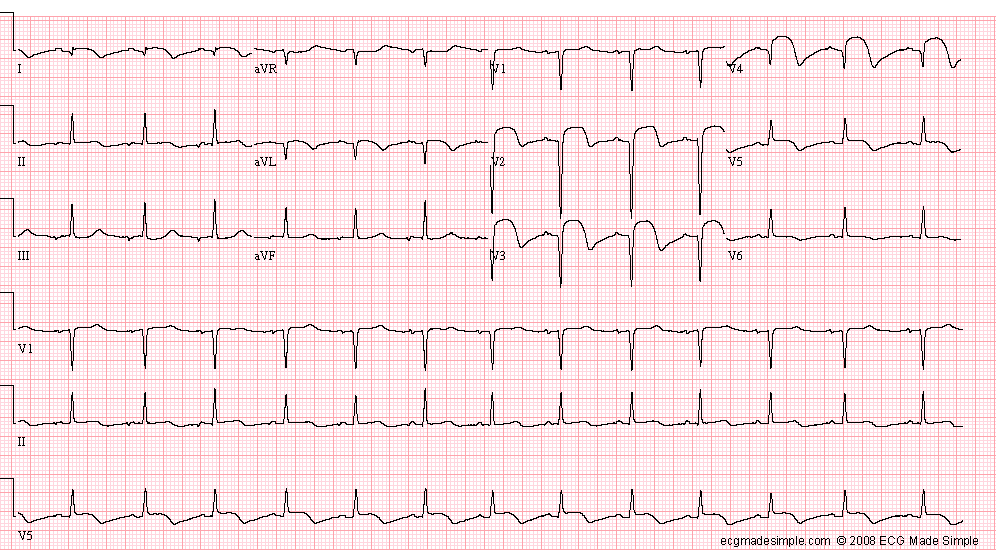
Case 102: A 32-Year-Old Man with Chest Pain
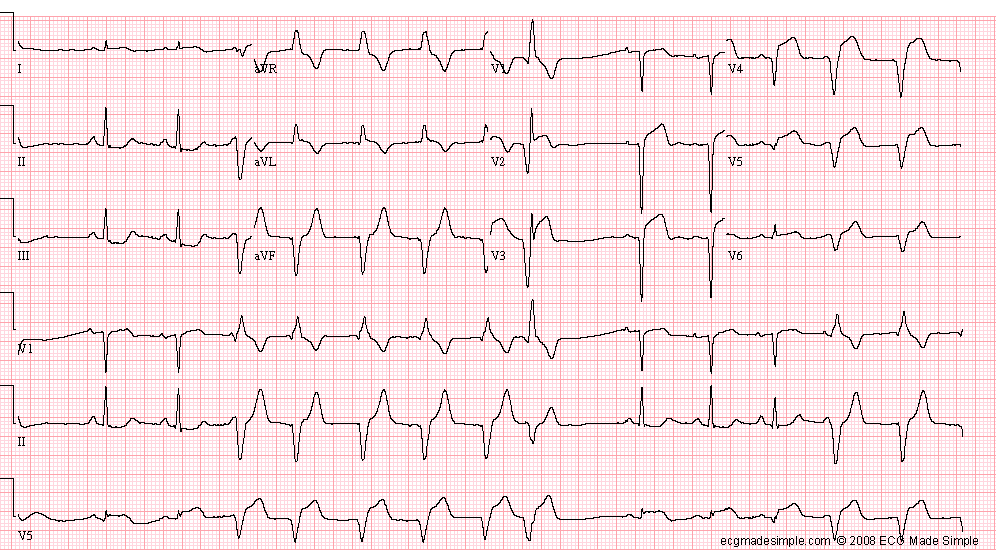
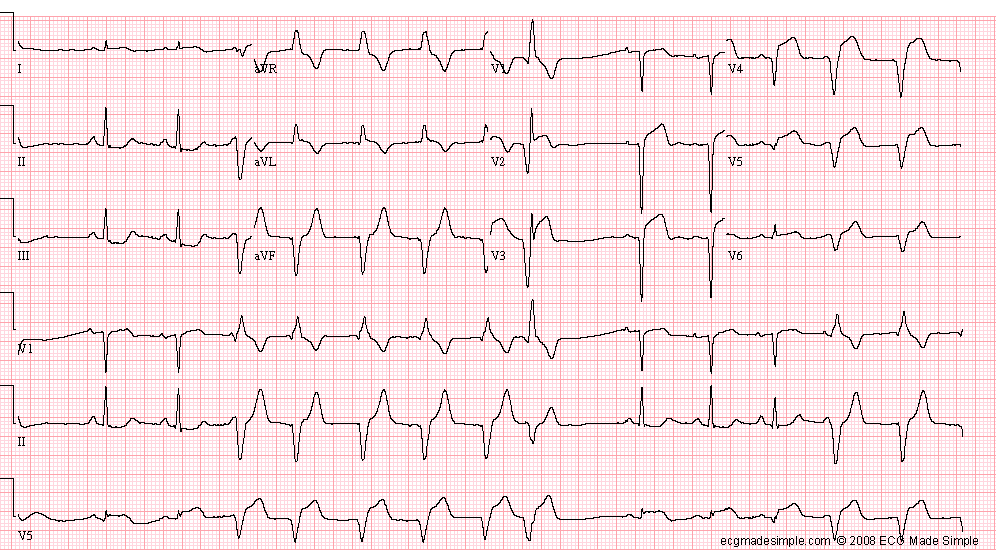
This 32-year-old man with several risk factors for coronary artery disease (family history, hyperlipidemia, and smoking) is seen in the Emergency Department one hour after the onset of severe retrosternal pain radiating to the left arm, associated with dyspnea and diaphoresis: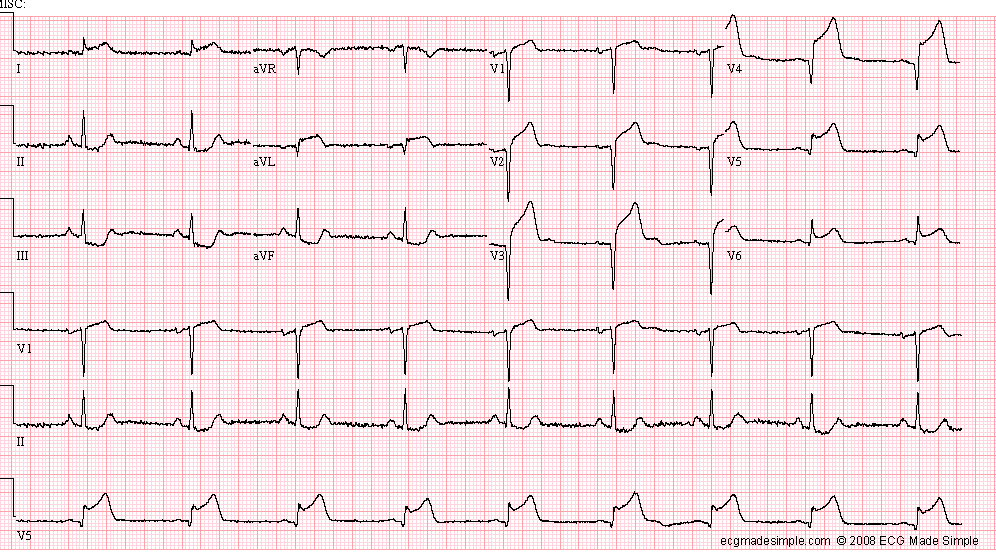
- Sinus bradycardia, 52/min
- Acute anterolateral infarction
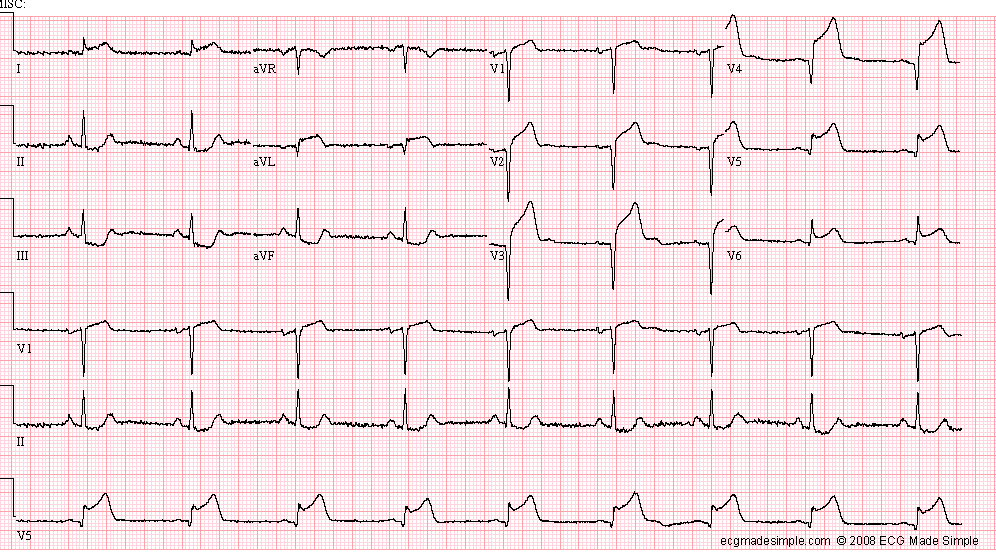
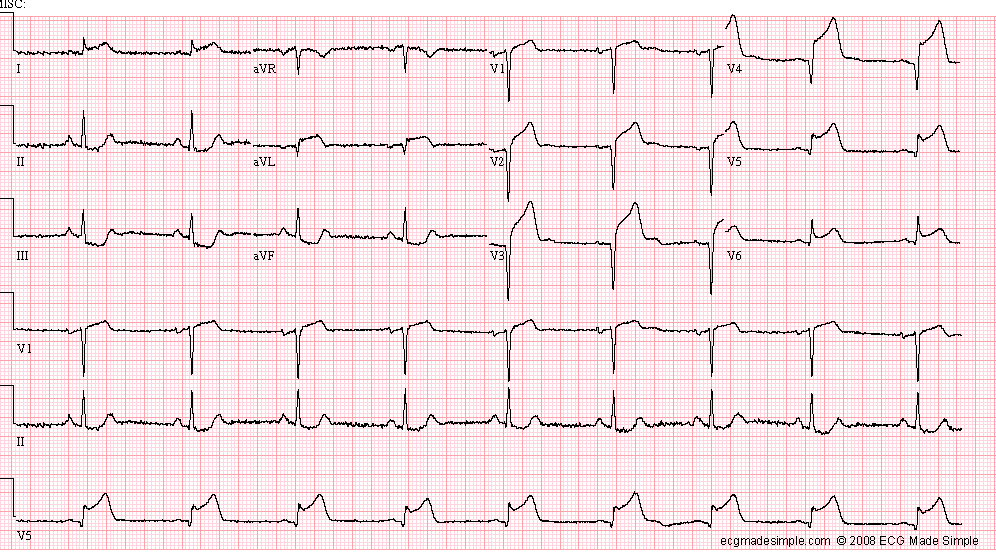
The patient is taken to Cardiac Catheterization Laboratory, where total occlusion of the left anterior descending artery (LAD) and 70% stenosis of the circumflex artery is identified. The LAD occlusion is crossed with a guidewire, the thrombus aspirated, and the stenosis stented. It was felt that the circumflex artery stenosis might be dilated at a later date, if indicated. The following ECG is recorded shortly after the procedure: 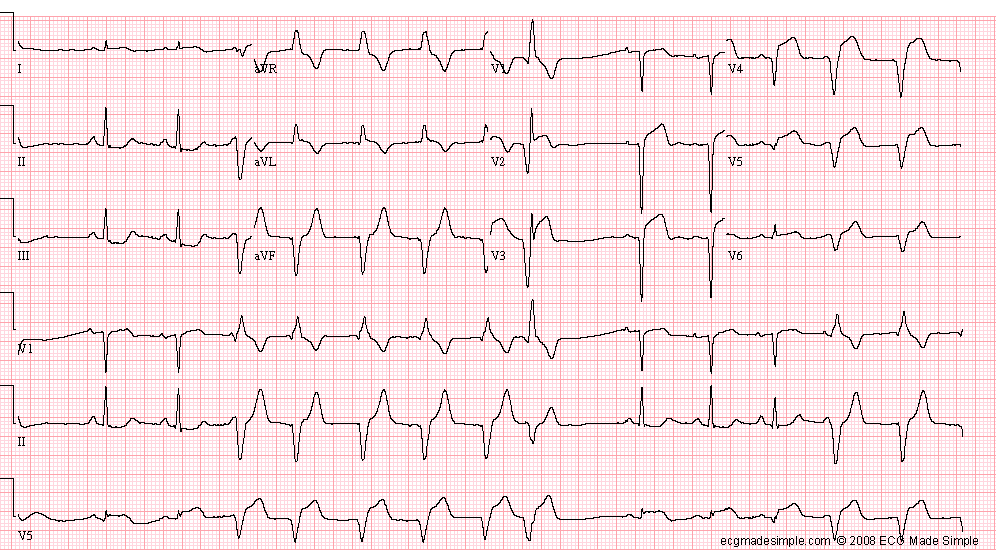
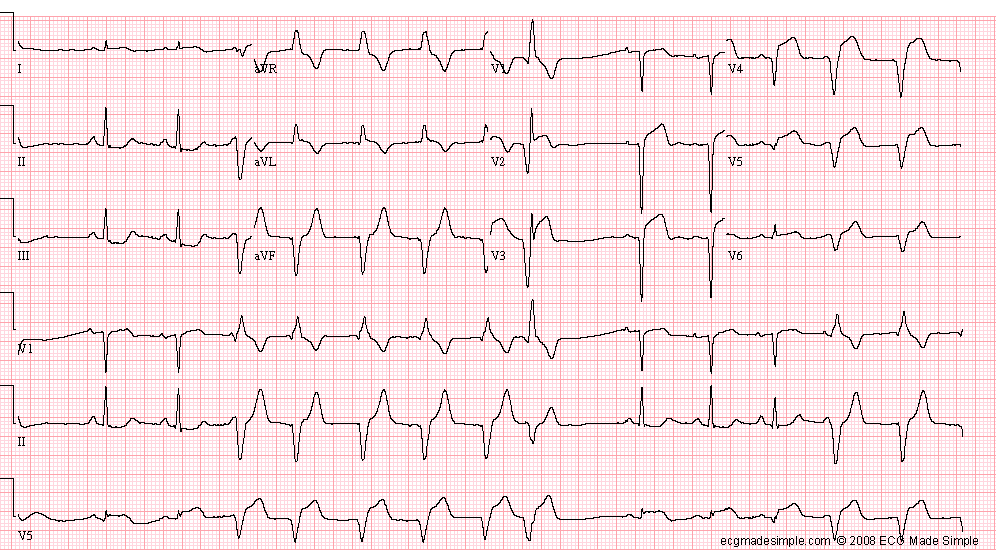
- Sinus rhythm with a competing accelerated idioventricular rhythm
- One premature ventricular complex
- Acute anterior infarction
Accelerated ventricular rhythms are common following reperfusion.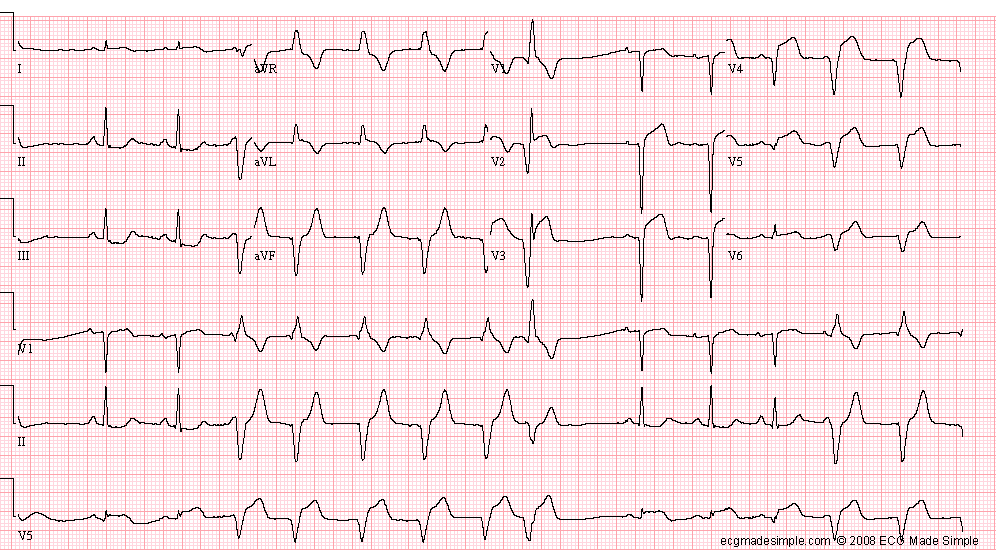
The following ECG is recorded nine hours after the angioplasty: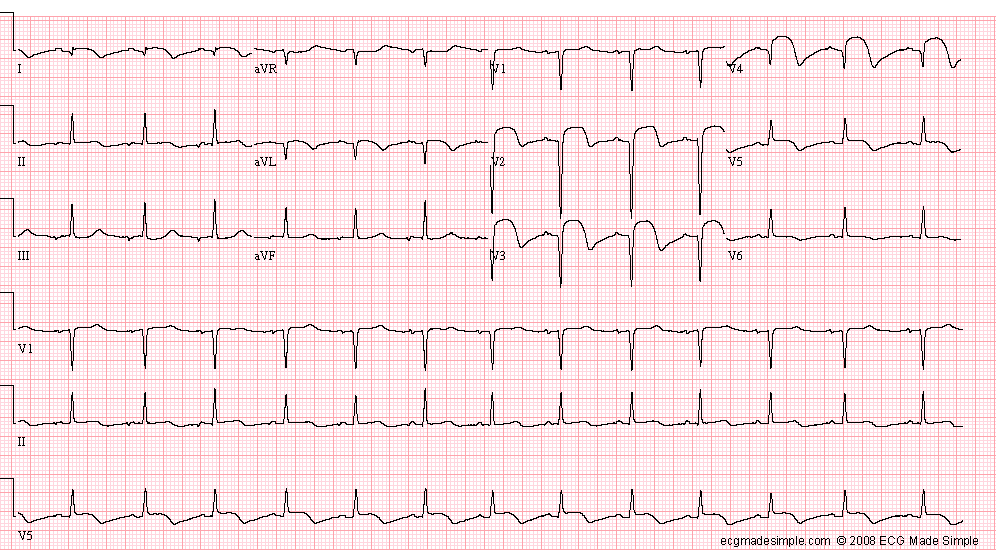
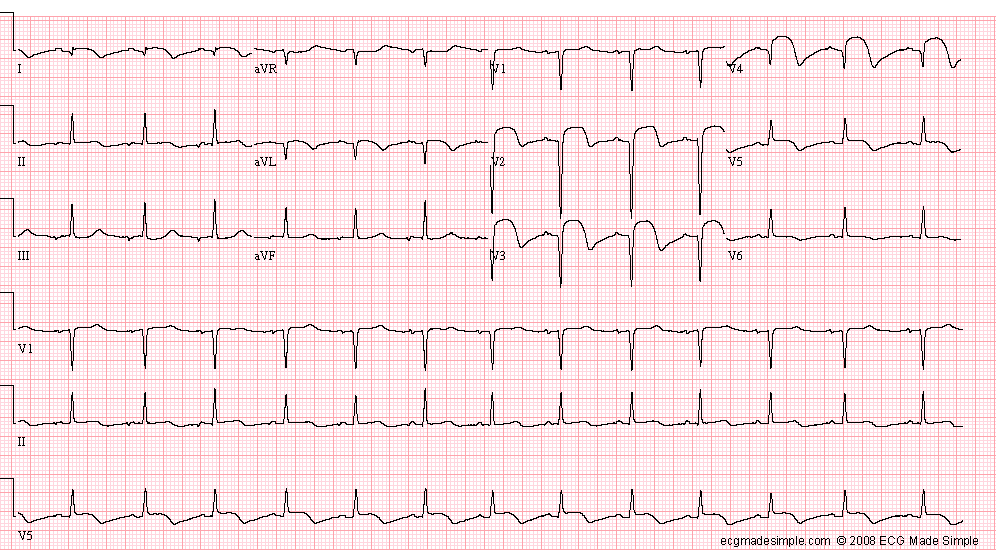
- Unusual P axis (negative P in II, III, aVF), probably ectopic atrial rhythm, 72/min
- Acute anterolateral infarction
The patient was in pulmonary edema during the angioplasty procedure. He was vigorously treated, and the signs of heart failure subsided. The serum troponin was >95, the CK 9,500. The echocardiogram demonstrated extensive wall motion abnormality, with an LVEF of 35% The condition of the patient became stable. He was free of chest pain and dyspnea. He was discharged after one week in satisfactory condition.
ECG ID: E436