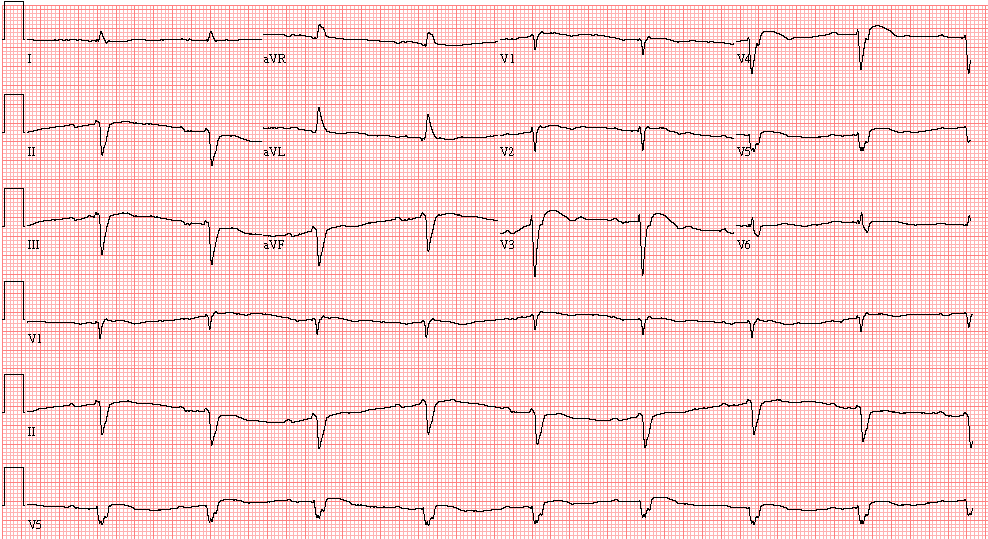
Case 19: A 67-Year-Old Man in Congestive Heart Failure
This 67-year-old man is admitted because of congestive heart failure due to ischemic cardiomyopathy. Ten years ago he had a myocardial infarction complicated by episodes of ventricular tachycardia, for which he received an ICD (Implantable Cardioverter Defibrillator) implant. His cardiac function had recently severely deteriorated, despite optimal therapy, with LV ejection fraction 26% and class III-IV NYHA HF:
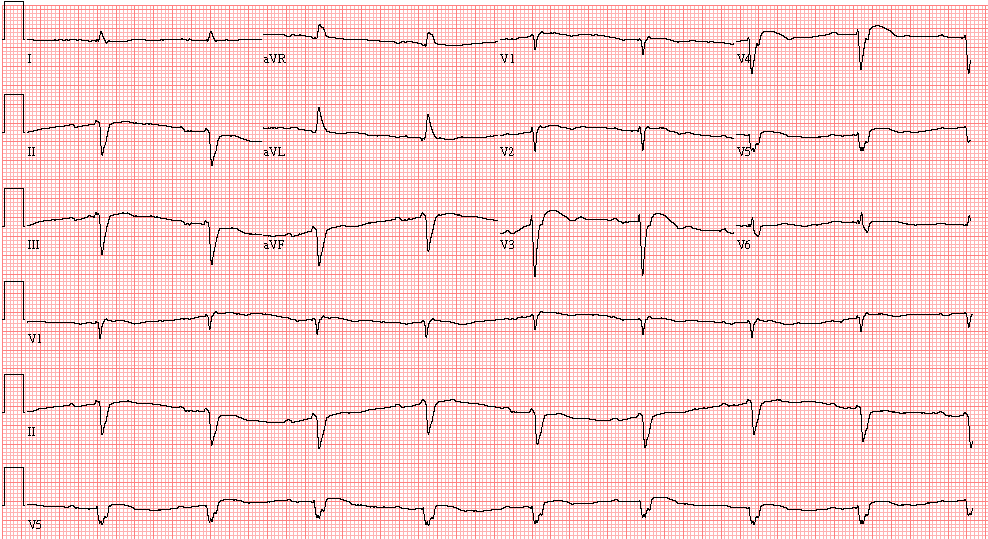
- Sinus bradycardia, 52/min.
- First degree AV block (PR=270 msec.)
- Left axis deviation
- Nonspecific intraventricular block – QRS duration 170 msec.
- R wave regression from V3 to V5 – Possible anterior infarct, age undetermined
The patient is referred to the EP Service and a procedure is carried out:
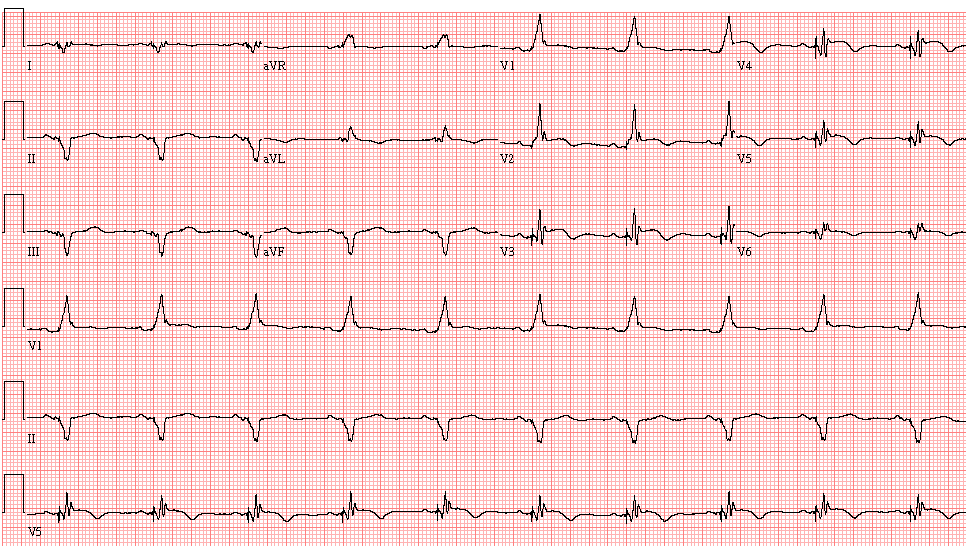
- Sinus rhythm, 60/min
- DDD pacing (atrial sensed, ventricular paced rhythm)
- Right superior axis deviation
- Broad R wave in V1 and V2 (right bundle branch block pattern)
- The QRS axis and pattern are suggestive of a biventricular pacemaker
Comment: The patient had an upgrade from single-chamber ICD (right ventricle) to ICD plus dual chamber CRT (pacing leads in both ventricles). The tip of left ventricular lead was positioned in a posterolateral coronary vein. CRT (Cardiac Resynchronization Therapy) achieved by simultaneously pacing both ventricles (biventricular pacing) has been proven to produce clinical benefits and to improve survival in patients with heart failure, low LV ejection fraction and intraventricular conduction delay.
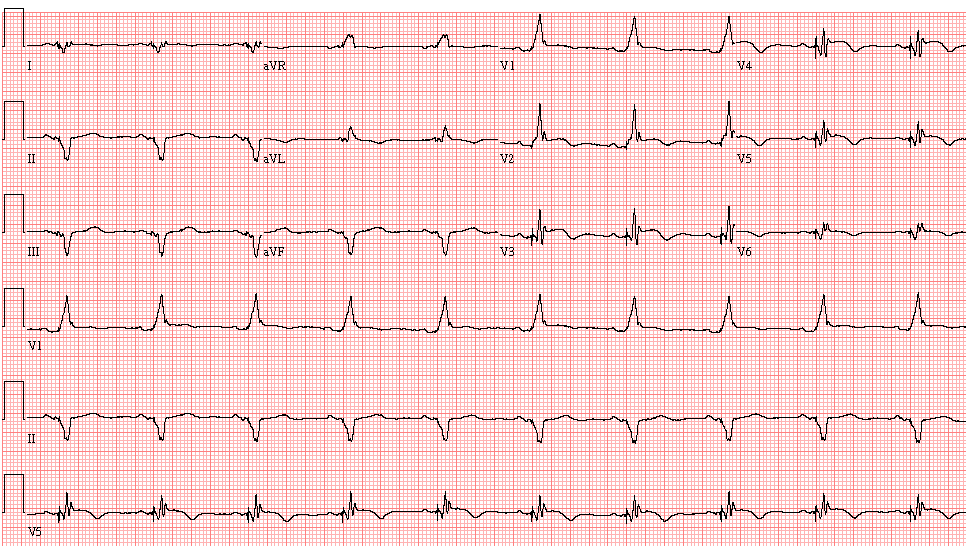
ECG ID: E640